Published by: Administrator

Some things we’re going to talk about today and then talk about the importance of verifying benefits, especially with Avid network patients, talk about financial agreements and our office policies, and talk about our claim creation and submissions, our patient cost sharing and what that means. The new No Surprises Act of 2022. How payers are handling out-of-network claims with the No Surprises Act of 2022? How patient involvement and communication can be helpful and important? And then, we absolutely will leave some time for questions at the end. So if you’ve got questions that come up out during the webinar, make sure you write them down. Also, if you could, please be specific if you’ve got a claim question, make sure you give me their CPT code, care specifics, whatever you can give me so that I can make sure I answer your questions as accurately as I can.
Also, I will have my email address on the last slide. You’re welcome to email your questions if they are really specific and you’d rather just send those offline, that’s completely fine as well. So I’ll try to leave at least 10 minutes for questions at the end. And then if we’re not able to get to all the questions, again, just go ahead and email me those and I will get back to you.
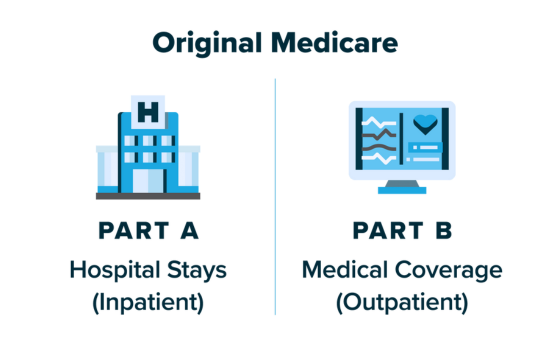
So let’s talk about the difference between in-network and out-of-network. Obviously, in – when we’re in- network with insurances, patients can seek us out. The insurances can even send patients our way, because they may call their insurance and ask for a recommendation of a doctor in their network. We might have a greater volume of patients, but we may have a lower reimbursement because of a contract that we may have. There’s a specific fee schedule that we’re paid off of that is agreed upon by the insurance company, usually not something that we can have anything to do with at this point.
[....]